The post Tending to Tendinitis appeared first on The New Straits Times
“A painful condition, there are things you can do to stop it from affecting your quality of life”, writes Aznim Ruhana Md Yusup

Repetitive actions like tending to your garden every day may lead to overuse of the tendon.
IN our bid to be in good physical shape, we are, at time, guilty of doing too much, too soon. So instead of becoming fitter and healthier, we end up being impaired by pain and injury.
This happens when we overestimate what our body can do. Age may be a number in our mind, but the physical wear and tear as you get older is too real to ignore. That pain in your shoulder or knee is also too real to ignore.
What could be happening here is tendinitis, which is the inflammation of the tendon. A tendon is a tissue that connects muscle to bone, helping to move the bones and joints when the muscles contract.
“But the tendon is what we call a watershed area, the blood supply there is not very good. If you do strenuous activity, what might happen is that your tendons go through overuse, which causes the inflammation.”
“It is something that happens to young people too,” Dr Tai continues. “But younger people can recover faster. At 40 or 50, the blood supply gets worse so you don’t always recover.”
Tendinitis can occur in any tendons in the body but most often in the elbow, wrist, shoulder, knee and ankle. It’s generally referred to by the body part involved or the activity that caused it. So, for example, if you play basketball a lot, you might have patellar tendinitis or jumper’s knee.
Daily repetitive actions like using a computer mouse, or in Dr Tai’s case, holding a scalpel to operate on patients, can also lead to tendon overuse. Acute injury that damages the tendon is another cause of tendinitis.

“Regular exercise will help get your muscles and tendons in the right shape so you won’t get this problem later on.” Dr. Tai Cheh Chin
LOOK TO R.I.C.E
When people have tendinitis, they usually complain about pain. “So if I have patellar tendinitis, every time I play basketball, my knees hurt. But when I walk, it is not that bad. This is because the stress you put on the knee when you walk is different. When you’re jumping and when you land, it puts more stress on the tendon.”
Dr Tai explains that the pain comes in stages, so it might be mild at first. It might not even be immediate, with the physical hurt only occurring the next day. But the tendinitis becomes more serious when it starts to hurt as you’re doing the activity. And it’s at its worst when it hurts even when you’re not doing anything at all.
For some people, tendinitis can appear as swelling. According to Dr Tai, this is typical of the four signs of inflammation; Pain, swelling, redness and heat, although in this case, redness and heat are not as common.
Treating tendinitis boils down to R.I.C.E. “R stands for rest. If you play badminton and you get tendinitis in your shoulder, then you should stop playing for a while. If you have a wrist tendinitis, wear a wrist brace or splint to hold it in its place. So you rest and protect the area and don’t do anything to aggravate the injury.”
The I stands for ice. This is because inflammation generates heat, so you need ice to cool it down and reduce further damage.
C is for compression, because of the swelling. And E is elevation, as you might need to elevate the affected area so that there would be less swelling.
Dr Tai has added P to the list, which stands for painkillers. “And it’s a group of painkillers known as anti-inflammatory tablets. They don’t directly reduce the pain but they are anti-inflammatory. If you reduce the inflammation, you reduce the pain.”
“Another thing that I ask the patient to do is physiotherapy. There are different modalities that can help you reduce the pain and the swelling.”
If that doesn’t work then Dr Tai would consider a steroid injection to the area. It’s effective but there is fine line that doctors need to tread between reducing the inflammation and possibly causing harm to the patient.
“If you use steroid injections too many times, it can cause ruptures of the tendon. Steroid can potentially weaken the tendon, the bone and the muscle. In rare occasions, the bone can become dead as a result of repetitive steroid injection.”
If you play sports regularly, you should warm up before your session.
WARM UP
While older folk are more likely to suffer from tendinitis, there is no link between males or females being more prone to the condition. “Anatomically, there’s no real advantage or disadvantage whether you are male or female. Female patients that I see tend to get tendinitis on the wrist because of housework.”
“If men get tendinitis on the wrist, they’re usually gardeners. There are certain types of activities that women do more than men that cause tendinitis, and vice versa. So it’s related to the activities that they do, rather than gender.”
Dr Tai’s advice is to rest and look after yourself the moment you spot the early signs of tendinitis. And if you play sports regularly, you should warm up before starting your session. “Regular exercise will help get your muscles and tendon in the right shape so you won’t get this problem later on. But don’t over-exert yourself.”
“If you’re over 40 or 50, don’t start doing marathons if you haven’t been doing it earlier. At 25, you can play 10 games of badminton. But at this age, it will hurt you.”
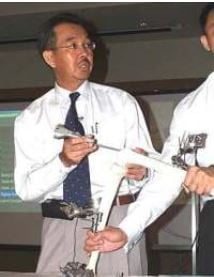
OSC Consultant Orthopaedic Surgeon, Dr Chan Kin Yuen, speaks on the topic of ‘The Management of Common Sports Injury‘ at the Myanmar Sports Science and Sports Medicine Conference.
About OSC:
Orthopaedic Specialist Centre (OSC) is the brainchild of four highly-experienced Malaysian orthopaedics specialists, who have come together to create an innovative centre of excellence purely focused on bone and joint care. Using their decades of experience in practice, they have embarked on a new mission for Malaysian orthopaedics. At OSC, the patient’s journey from treatment to recovery is accompanied by elevated levels of personalised expertise and empathy, in order to make a real difference to our patients’ lives. In contrast to large, faceless hospitals, OSC is a uniquely intimate medical boutique, one that puts meticulous, tailored care at the heart of the patient experience. OSC aims to redefine orthopaedics care in Malaysia, by making world-class treatment comfortable, cost-effective and attainable for the whole community. For more information, please visit www.oscortho.my

The post Regaining Pain-Free Motion appeared first on The Star.
LIVING with severe osteoarthritis in the knee is painful and debilitating. However, with total knee replacement (TKR) surgery, you could regain quality of life.
Datuk Dr Lim Boon Ping, consultant orthopaedic surgeon at Subang Jaya Medical Centre, says, “TKR is a common surgery performed on elderly patients. It involves opening the knee joint, resurfacing the worn, painful joint with a metal alloy and using a high-density polyethylene (plastic) between the surfaces of the joint.”
However, he notes that TKR is suggested only to those with severe osteoarthritis, and not mild or moderate cases. It is advised only as a last resort after it is determined that painkillers and lifestyle modifications have failed to reduce the pain in the knee when conducting daily activities.
Clear expectations
Before proceeding with TKR, it is important for a patient to understand the full procedure and what to expect before, during and after surgery.
Dr Lim summarises, “Before surgery, the doctor will explain the procedure and risks involved. The patient’s history of illnesses and allergies are discussed and managed, to reduce risks before admission for surgery.”
X-rays of the knees, an assessment of the patient’s
suitability to go under anaesthesia and blood tests for underlying medical conditions are performed during preparation for surgery. In addition, patients are asked to fast six hours prior to surgery. The surgery takes between one and two hours and is performed through an anterior (front of the knee) incision.
Dr Lim continues, “After surgery, a physiotherapist will guide the patient through lowerlimb exercises and, subsequently, walking, the very next day. The patient is encouraged to use his full body weight on his lower limbs and bend and stretch the knee as much as he can. The more this is done, the faster his recovery. Thus, a patient with better pain control who moves and exercises his knee and ankle more frequently will recover faster.”
After the patient is able to walk well with a walking frame, he will be discharged from the hospital. He will still be required to undergo follow-ups as determined by his doctor and continue physiotherapy exercises at home to ensure smooth recovery.
Walking through life anew
After TKR, Dr Lim states that almost all patients should be able to walk long distances, jog, cycle and climb hills or stairs with ease and painlessly within three to four months.
There is also no need to worry about the longevity of your new knee. He says, “The replaced knee usually lasts around 25 years with normal usage for a patient of average weight. While there are risks with this surgery, the probabilities of occurrence are only 0.5% for infections, 0.001% for deep-vein thrombosis leading to pulmonary embolism and 20% for residual mild pain and weakness that do not require analgesics or painkillers.”
TKR is a relatively low-risk surgery with a high success rate and not only gives you the ability to walk painlessly again, but also a new lease on life.
For more information, call 03-5639 1212.
The article One patient, one implant appeared first on The Star.
“It’s a new revolution in knee replacement surgery,” says consultant orthopaedic surgeon Dr Tai Cheh Chin

In traditional knee implant surgery, the knee is shaped to fit the implant, not the other way round.
The “revolution” he’s speaking of is the ConforMIS knee replacement system, which offers unique advantages over traditional, off-the-shelf implants in knee replacement surgery.
“Traditionally, with knee replacement implants, we try to shape and cut the knee so that it fits the implant,” says Dr Tai.
“The patient can be male, female, bigger or smaller in size, it makes no difference – we cut the knee in the same pattern because the implant shape and size is always fixed.
“Traditional implants do not take into account the differences in knee anatomy between man, woman, Asian, Causcasian, African… You fit the knee to the implant,” he adds.
“Everybody’s knee is different,” Dr Tai goes on. “All the data’s there. A simple example – an Asian knee vs a Western knee. We cut the knee depending on data from Western populations, and that’s a problem as our sizes are different, our shapes are different; so if size, shape and alignment are different, then how can we have an implant that can fit nicely?
“So you find that in knee replacement surgeries, no matter how good a surgeon you are, for about every five knees that you operate on, one patient – even though the implant looks perfect on x-rays – will not be vey happy with the results.
“The first modern knee implant was carried out in the 1970s in the United States; the shape has not changed that much, though improvements have been made over the last 10-20 years.
“We have computer navigation to put in the implant better; to cut the knee better, we have PSI – patient specific instrumentation – where we make it more patient specific, but in the end, we still have to use that standard implant. We have focused the tech on how to cut the knee better, but the implant basically remained unchanged,” says Dr Tai.
The new system allows for patient-specific fitting of the implant, which means no implant is alike because it has been made to fit only one particular patient.
“With the system, you first CT the knee. This information is then sent to the United States, where 3D modelling of the implant is carried out according to the specifications measured from the knee CT scan.
“During this time, the surgeon will be kept informed of developments to make sure everything required is being carried out.
“Once both parties agree to the specifications, the 3D implant is made. The implant will then be delivered to the surgeon a few days before the date of surgery.
“The whole process, on average, takes between four and six weeks,” says Dr Tai.

According to Dr Tai, this system is designed to follow the contour of each patient’s anatomy, resulting in much better fit and less complications.
An analogy, says Dr Tai, can be made with buying shoes. Rather then getting general sizes, such as 7, 8 or 9, you get the shoe custom-made for you, which naturally makes it a better fit and it will be much more comfortable than off-the-shelf shoes.
This system has been available in the United States for more than 10 years.
“In the US, the first such implant was carried out in 2004, so it has been more than 10 years. We have more than 10 years’ worth of data now, and it reflects the many advantages of this ‘new’ system,” notes Dr Tai.
One advantage of the system is that you can replace whatever portion (of the knee) that you want to.
“Unlike the traditional knee replacement, where you only have the option of partial, half-knee or total replacement, this system allows you to replace any part that is damaged. You get to keep the good parts of the knee,” explains Dr Tai.
This advantage has far-reaching implications. People getting knee replacement surgery are getting younger, so the possibility of a revision of the implant is higher. So when it’s time for a revision, such patients may still have functional parts that don’t have to be replaced.
Another plus for the system is instrumentation, which makes the surgery itself faster and easier.
“This system makes the whole knee replacement operation easier. With traditional implants, there are about eight trays of instruments in the op theatre because we don’t know what size implant to use. We need to cut open the knee and then assess the size of the implant.
“With the new system, it’s just one box,” says Dr Tai.
According to Dr Tai, studies have shown that with the new system, knee alignment accuracy is a lot better. The resulting knee kinematics is almost like normal, hence 90% of patients say their knee feels like normal (because it’s shape is good, it fits well and the kinematics are very good), compared to traditional knee replacement implants where 60-70% say their knees feel quite normal.
“Outcomes are good – shorter hospital stay; less blood loss as operating time is shorter; reduced complication rates. So although this implant is more expensive, in the short term, with shorter hospital stay, less complications, less blood loss, less revisions, you save a bit more,” notes Dr Tai.
Today, on average, US surgeons carry out approximately 4,000 to 6,000 knee replacement surgeries using this system.
“With this, we expect patients to be happier with the results. Finally, we get an implant that fits the patient, rather than requiring the patient to fit the implant; that’s the biggest change,” says Dr Tai.
[pdfjs-viewer url=”https%3A%2F%2Fwww.oscortho.my%2Fwp-content%2Fuploads%2F2017%2F09%2Fitotal-Sept-2017.pdf” viewer_width=100% viewer_height=800px fullscreen=true download=true print=true]
“Rather than an off-the-shelf knee implant that requires the surgeon to shape the knee to fit the implant, this implant is custom-made to fit the patient.”
The post A Knee Implant Just For You appeared first on The Star.
The next step forward for knee replacement implants is here, and it offers customised implants built specifically to the measurements of each patient.
“IT’S a new revolution in knee replacement surgery,” says consultant orthopaedic surgeon Dr Tai Cheh Chin.
The “revolution” he’s speaking of is the ConforMIS knee replacement system, which offers unique advantages over traditional, off-the-shelf implants in knee replacement surgery.
“Traditionally, with knee replacement implants, we try to shape and cut the knee so that it fits the implant,” says Dr Tai.
“The patient can be male, female, bigger or smaller in size, it makes no difference – we cut the knee in the same pattern because the implant shape and size is always fixed.
“Traditional implants do not take into account the differences in knee anatomy between man, woman, Asian, Causcasian, African… You fit the knee to the implant,” he adds.
“Everybody’s knee is different,” Dr Tai goes on. “All the data’s there. A simple example – an Asian knee vs a Western knee. We cut the knee depending on data from Western populations, and that’s a problem as our sizes are different, our shapes are different; so if size, shape and alignment are different, then how can we have an implant that can fit nicely?
“So you find that in knee replacement surgeries, no matter how good a surgeon you are, for about every five knees that you operate on, one patient – even though the implant looks perfect on x-rays – will not be vey happy with the results.
“The first modern knee implant was carried out in the 1970s in the United States; the shape has not changed that much, though improvements have been made over the last 10-20 years.
“We have computer navigation to put in the implant better; to cut the knee better, we have PSI – patient specific instrumentation – where we make it more patient specific, but in the end, we still have to use that standard implant. We have focused the tech on how to cut the knee better, but the implant basically remained unchanged,” says Dr Tai.
The new system allows for patient-specific fitting of the implant, which means no implant is alike because it has been made to fit only one particular patient.
“With the system, you first CT the knee. This information is then sent to the United States, where 3D modelling of the implant is carried out according to the specifications measured from the knee CT scan.
“During this time, the surgeon will be kept informed of developments to make sure everything required is being carried out.
“Once both parties agree to the specifications, the 3D implant is made. The implant will then be delivered to the surgeon a few days before the date of surgery.
“The whole process, on average, takes between four and six weeks,” says Dr Tai.
An analogy, says Dr Tai, can be made with buying shoes. Rather then getting general sizes, such as 7, 8 or 9, you get the shoe custom-made for you, which naturally makes it a better fit and it will be much more comfortable than off-the-shelf shoes.
This system has been available in the United States for more than 10 years.
“In the US, the first such implant was carried out in 2004, so it has been more than 10 years. We have more than 10 years’ worth of data now, and it reflects the many advantag- es of this ‘new’ system,” notes Dr Tai.
One advantage of the system is that you can replace whatever portion (of the knee) that you want to.
“Unlike the traditional knee replacement, where you only have the option of partial, half-knee or total replacement, this system allows you to replace any part that is damaged. You get to keep the good parts of the knee,” explains Dr Tai.
This advantage has far-reaching implications. People getting knee replacement surgery are getting younger, so the possibility of a revision of the implant is higher. So when it’s time for a revision, such patients may still have functional parts that don’t have to be replaced.
Another plus for the system is instrumentation, which makes the surgery itself faster and easier.
“This system makes the whole knee replacement operation easier. With traditional implants, there are about eight trays of instruments in the op theatre because we don’t know what size implant to use. We need to cut open the knee and then assess the size of the implant.
“With the new system, it’s just one box,” says Dr Tai.
According to Dr Tai, studies have shown that with the new system, knee alignment accuracy is a lot better. The resulting knee kinematics is almost like normal, hence 90% of patients say their knee feels like normal (because it’s shape is good, it fits well and the kinematics are very good), compared to traditional knee replacement implants where 60-70% say their knees feel quite normal.
“Outcomes are good – shorter hospital stay; less blood loss as operating time is shorter; reduced complication rates. So although this implant is more expensive, in the short term, with shorter hospital stay, less complications, less blood loss, less revisions, you save a bit more,” notes Dr Tai.
Today, on average, US surgeons carry out approximately 4,000 to 6,000 knee replacement surgeries using this system.
“With this, we expect patients to be happier with the results. Finally, we get an implant that fits the patient, rather than requiring the patient to fit the implant; that’s the biggest change,” says Dr Tai.
Dr Chan Kin Yuen, President of the Malaysian Association of Sports Medicine, talks about his experience working with Medical Conference Partners (formally known as Bloom Communications) during the 1st ASEAN Sports Medicine Conference 2015.
Running is a common cause of sports injuries.
The original article can be found at The Star: https://www.thestar.com.my/lifestyle/health/fitness/2012/11/11/running-scared
RUNNING is a simple and convenient sport that makes it a popular form of exercise. It lowers the rate and progression of disability, risk to chronic diseases, and mortality rates.
However, runners are also exposed to the risk of injuries. The common injuries sustained are mostly due to overuse that usually heal without major intervention.
More serious injuries can lead to long-term consequences if precautions are not taken and appropriate treatment not started early.
Previous injuries and total running mileage seem to consistently predict running injuries. For example, it is estimated that serious distance runners, defined as those who run more than 25 miles (40km) a week, have an injury rate of about 30% per year.
There are many injuries associated with running, affecting different parts of the lower limb. About 25% affect the knee; 20%, the lower leg; 16%, the ankle; 10%, the upper limb; 7%, hips and pelvis; and 7%, the lower back.
A survey carried out in the US shows a differing pattern of injury between younger and older runners. Knee and shin problems appear to affect the young, while older runners more commonly sustain injury to the calf, Achilles tendon and hamstrings.
For the purpose of this article, meniscus injury that can lead to long-term arthritis of the joints will be discussed.
Meniscal tear
The knee is the largest joint in the body, and has many parts that perform different functions.
The menisci (medial and lateral meniscus) are thick rubber-like pads of cartilage tissue that act like shock absorbers in the knee joint. A meniscus can be torn, commonly after a forceful twisting injury to the knee.
Meniscal tears are one of the most common injuries that can occur from running. If left untreated, some may progress to osteoarthritis of the knee.
Meniscal tears can occur at any age, although the type of tears may differ. In the younger age group, tears are usually related to sports trauma from twisting injuries, while tears in the older age group tend to be due to age-related changes in the meniscus.
Often, there is a “pop” when the meniscus tears. If the tear is small, the symptoms are often minimal, with little effect on walking or running. There may be associated swelling, and often, full weight-bearing is painful, with reduced range of motion.
When large meniscal tears occur, they may cause catching, locking or sudden “giving way” while walking. This is a result of loose fragments that slip into the joint between the femur and tibia. These may act as loose bodies abrading the articular cartilage at the end of the femur and tibial surfaces.
Persistent abrasion will lead to loss of articular cartilage, and eventually, bone is exposed, leading to osteoarthritis when both bone surfaces of the femur and tibia scrape against each other, causing pain, deformity and reduced function of the knee.
Tenderness along the joint line and special examination on the knee may produce a clicking sound suggestive of a meniscal tear. An X-ray is often not conclusive, but is usually done to exclude bony loose fragments or other bone conditions causing similar symptoms.
MRI is most helpful in confirming the diagnosis, and more importantly, to check for other injuries to the articular cartilage on the femur and tibia that will influence treatment and any additional procedures required.
Often, if the knee is stable and the symptoms are not prolonged, PRICE management is all that is needed. PRICE stands for Pain control, Rest, Ice, Compression and Elevation.
Pain control can be managed by NSAIDs (nonsteroidal anti-inflammatory drugs), or a newer class of medications known as selective cox-2 inhibitors, which markedly reduces gastric and gut irritation and ulceration.
It is a common mistake to think of such drugs as pain control medication only. It is equally important to be aware that these drugs reduce pain by reducing the inflammatory process that occurs after any injury.
The ideal pain control medication should be one that acts fast, with effects that last a longer time.
Next is rest. This is often trivialised, but it is essential to give the injured meniscus adequate time to heal. As is often the case, healing is programmed in humans, but if the injured part is not rested, this will prolong the healing process beyond the average four to six weeks.
Crutches and non-weight bearing, and sometimes bracing the knee, allows it adequate rest for healing.
An elastic compression support would help to reduce the additional swelling and blood loss after injury, and also restricts the range of motion for pain relief.
In addition, ice is a simple and effective means of reducing swelling in an acute injury, but needs to be applied every 20 minutes at a time several times a day. Direct contact of ice to the skin continuously will cause cold burns, leading to more injury, so wrap the ice with cloth or a bag.
Lastly, elevation is often overlooked and is the simplest measure to reduce swelling by elevating the knee above the horizontal level of the heart.
When pain and swelling persists in spite of non-operative treatment, then surgery may be needed. Knee arthroscopy, a form of key-hole surgery, is one of the commonly performed knee procedures. It involves inserting a small video camera through a small incision into the knee joint. Another small incision is often used for inserting specialised small instruments. This provides an excellent view of the injury of the knee for close examination, and manipulation with a probe or treatment with other instruments.
Reparability depends on the size, location and type of tear. Occasionally, it is possible to trim some parts of the meniscus and repair some other parts with the aim of preserving as much of the meniscus as possible.
Trimming the meniscus probably increases the risk of osteoarthritis (with the loss of meniscus that does not grow back). However, the risk of articular cartilage damage from loose symptomatic meniscal fragments can be more damaging, leading to more rapid osteoarthritis changes. It is analogous to a stone inside a shoe abrading the sole of the foot, causing blistering and ulceration.
Other factors that need to be considered in the treatment of meniscal tears include age, activity level and occupation.
Rehabilitation of the knee after arthroscopic surgery is another often-ignored aspect that has a major bearing on the final result.
Early controlled rehabilitation is essential for optimal results. Occasionally, a knee brace is needed after surgery to prevent excessive movement.
During the healing process, controlled progressive range of motion and exercises to maintain muscle strength is necessary. When meniscal healing is complete, a full range of motion and strengthening programme is added.
Much of the rehabilitation programme can be done at home with simple resistive exercises with exercise bands that are cheap and lightweight.
Preventing injuries
Muscles, tendon and ligaments are important to support the knee. As such, muscle conditioning, as well as muscle, tendon and ligament flexibility, are important to prevent knee injury.
Muscle strength, endurance and balance training of the entire lower limb, and sustained gentle stretching of the hamstring and calf muscles, are important, as tightness of these muscles are common in runners.
Adequate warm-up and stretches before running is essential to prevent muscle, tendon and ligament injuries. It is equally important to cool down after running to enable the body to recover.
Proper running shoes are important to prevent injuries, particularly the foot. There are essentially three types of such footwear. A motion–control shoe is for a runner who needs more rigid support; a support shoe is for those who do not need much control; and a cushion shoe is for a runner with a rigid foot that requires flexibility and cushioning for shock absorption.
Adequate warm-ups is important to allow the body to prepare for the demands of intense running. It increases the blood flow to the muscles. This can be done with running at an easy pace at the beginning. The warming-up duration can vary, with those who are newer to running taking a longer time.
After warming the muscles, stretches need to be done to improve flexibility. Stretching cold muscles can cause injury. Stretches should probably best be done standing up at the start of the running session. Floor stretches should be carried out during the cooling down after running. This will allow the body to respond better and prevent injuries.
Stretches should be done slowly and gently to avoid muscle tension and pain, with each stretch held for 10 to 30 seconds.
The cooling-down phase at the end of running is to allow the body to recover effectively. It should start with a gradual decrease in running intensity at the end of the running session, and slowing down to a walk at a comfortable pace until breathing and heart rate returns to normal.
In summary, running is a healthy way to stay fit. With proper precaution and an adequate regular training programme, the risk of injury can be minimised. It is important to be aware that injuries may occur and that early intervention is advisable to prevent longer term disability.
This article is a collaborative effort by Dr Chan Kin Yuen together with MSD and is supported by the Malaysian Association of Sports Medicine. The information provided is for educational and communication purposes only and it should not be construed as personal medical advice. Information published in this article is not intended to replace, supplant or augment a consultation with a health professional regarding the reader’s own medical care. The Star does not give any warranty on accuracy, completeness, functionality, usefulness or other assurances as to the content appearing in this column. The Star disclaims all responsibility for any losses, damage to property or personal injury suffered directly or indirectly from reliance on such information.
The article Lack of infrastructure repels talent from returning appeared first on The Star.
PETALING JAYA: Malaysia faces an uphill struggle in convincing its million-strong diaspora, of which nearly 30% have some form of tertiary education, to return and share their knowledge and experience even as the country embarks on reforms to transform the economy and achieve high-income status by the end of the decade.
Speakers at the third session of the national conference on “Making a high-income nation a reality” identified the lack of infrastructure such as a decent education system, meritocracy and leadership as reasons why skilled Malaysians were not coming back.
The speakers were orthopedic surgeon Dr Tai Cheh Chin, Dynamic Search Sdn Bhd director Tricia Yeoh and Leaderonomics Sdn Bhd chief executive officer Roshan Thiran with Housing and Local Government Minister Datuk Wira Chor Chee Heung moderating.
Tai, who cited data that one of 10 medical doctors left the country, said there were not enough centres of excellence in the healthcare industry while research and development was lacking.
Tai said the Government needed to be more proactive in recruiting Malaysian talent from abroad. “When I was in Cambridge, no official approached me,” he added.
Yeoh, meanwhile, said the Government was not doing itself a favour when the good work done by the Performance Management & Delivery Unit and Talent Corp was overshadowed by lingering issues on ethnic-based policies.
“This will leave questions in the minds of the diaspora and make them more reluctant to come back,” she said, adding that the country had a very low return migration rate.
Yeoh said there must be a paradigm shift away from the ethnic-based policies to needs-based policies as there were inconsistencies in what the New Economic Model recommended and what certain agencies such as Teraju, set up by the Government to safeguard bumiputra business interests, stood for.
Roshan said talent was attracted to leadership and the infrastructure that developed leaders. “The heartbeat of leadership is the constant upgrading of skills. Leaders are made through experience,” he said.
The article Joint Health appeared first on The Star.
WHEN I get older, losing my hair, many years from now? Will you still need me? When I’m sixty-four?… Yours sincerely, wasting away” – When I’m 64 by The Beatles
Poignant lyrics by The Beatles from way back in 1967. Fast forward to 2005 and we are looking at 73 years or even 100 years by 2030! I am sure it comes as no surprise that we are living longer today – at last count in Malaysia we were averaging 73 years.
Older people today are challenging the stereotype that old age means vulnerability and incapacity to make decisions. We are stronger, bolder and demanding more of ourselves in every way. This is helping to develop a new account of ageing, that of the “heroic third ager” who is more and more living the life of the younger generation than that of the “old and vulnerable elder”.

Improving joint alignment has been a focus of surgical technique research and development and computers have been roped into the surgery room to help surgeons better ‘see’, ‘find’ and ‘place’ throughout.
However, there’s no denying the physiological decline of the body as we age. As a doctor, I face every day what is emerging as the most feared threat to living large in our golden years – joint degeneration.
Although very much a disability of the body, the impact that joint diseases have on the ability to walk and function without help over time amplifies its effects to the mind, heart and soul.
Any joint disease, whether inflammatory, degenerative or post-traumatic, will ultimately lead to erosion of cartilage and joint damage if the condition is left to progress untreated. This will culminate in swelling, pain, deformity and instability of the joint.
A majority of minor joint problems respond well to first line treatment – physical therapy, medication, and injections. However, more serious conditions may require a higher level of treatment. In these severe situations, surgical reconstruction can be a real treatment option, dramatically improving independence and quality of life by relieving pain and improving mobility.
One of the most effective treatment is total joint replacement or total joint arthroplasty (TJA). TJA can improve joint problems associated with severe injury to the joint, osteoarthritis, rheumatoid arthritis, and other degenerative conditions such as osteonecrosis – a condition in which obstructed blood flow causes bone tissue to die.
You’ve come a long way, baby
Since “invented” by Sir John Charnley, an orthopaedic surgeon at Wrightington Hospital for Joint Diseases in Wigan, England in 1961, TJA has come a long way. It has become fairly routine and is successful around 95% of the time. Minimally invasive surgery (MIS) techniques, instrumentation for better alignment and advancement in prostheses design and materials have all contributed to making the total surgical experience and results of TJA, notably for the hip and knee, the best it has ever been with survival rates of over 90%.
The main goal of TJA is the return of mobility and function. All you DYI enthusiasts will know that precise alignment of hinges is the key to optimising the function of moving parts. In the case of TJA, the hinge is your joint! Improving joint alignment has been a focus of surgical technique research and development, and computers have been roped into the surgery room to help surgeons better “see”, “find” and “place” throughout.
The precise alignment of hinges is the key to optimising the function of moving parts.
This technology, also called computer-assisted surgery (CAS), uses the same positioning technology as that fitted in cars to help you navigate streets – global positioning system or GPS. It helps the surgeon make the right cut and align the artificial joint to the bone more precisely for each individual patient.
CAS has been shown to increase the effectiveness of joint replacements and offers substantial benefits to the patient including a more rapid return to previous activity levels as well as durability of the prostheses thereby preventing the need for repeat surgery.
In most instances a joint replacement should last at least 15 years or longer. This revolutionary surgical technique is an option readily available in Malaysia today and with an estimated 20,000 patients considering TJA annually, CAS can offer a real treatment option that is simpler, safer and with better results.
The right treatment for the right patient
Are you a right candidate for joint replacement surgery? This is a conclusion you need to reach with the counsel of your surgeon who will take into consideration:
- The severity of your condition and how much it limits your mobility and function
- The risk of further injury if you don’t have the surgery
- Overall good health
- Failure to respond to conservative treatment Equally important, as a patient you need to consider:
- Your lifestyle including how much exercise you get
- Your willingness to modify and adapt your lifestyle to either option
- Your motivation to work through rehabilitation to strengthen your joint after surgery.
Complications of total joint arthroplasty
No surgery is without risk, similarly TJA. Complications may include infection, joint instability, joint stiffness, deep vein thrombosis and anaesthetic problems. Your surgeon will assess you pre-surgery to make sure you are able to withstand the surgical procedure. He or she will also ensure that you fully understand the limitations and risks of the procedure before consenting to the operation.
Walking down the road of life
As we see ageing as a destination rather then an end, we are shaping our approach to preventative medicine and forging new breakthroughs in medical treatment to give older persons the ability to live life longer and better.
TJA remains one of the most successful and effective procedures in surgery with a success rate of over 95% in leading medical centres. Patients are most impressed with the immediate relief of pain and discomfort. They can look forward to walking within two to three days and are discharged from the hospital after four to five days. With improving surgical techniques and instrumentation including CAS and minimally invasive approaches, the day will come when joint replacement is done on a day care basis.
Note: Dr Lee Chong Meng is a consultant orthopaedic and arthroplasty surgeon.
The post My foot … care appeared first on The Star.
THE foot is a complex anatomical structure tailored to withstand the demands of being the organ of locomotion of the human being. It consists of 26 bones, various interlocking ligaments and multiple tendon slings all cushioned by specialised tissues of the sole.
This complex combination allows the foot to adapt to the infinite demands placed on it during the various activities of daily living. But it is also this complexity that makes it vulnerable to injuries and ailments. Conditions of the foot that may need medical attention include traumatic, degenerative, inflammatory and infective problems.
Traumatic injuries to the foot are a common presentation to the orthopaedic specialist. Acute ankle and foot sprains are normally treated with cold compresses, rest, elevation and compression bandaging. Medication is needed for pain relief.
Fractures of the ankle and foot are not uncommon. Ankle fractures can be complex and may need surgical intervention, especially for those involving the ankle articulation. Neglected fractures can lead to rapid ankle joint degeneration, as the ankle mortise does not tolerate even minor incongruity.
Fracture of the 5th metatarsal base is very common and is normally treated conservatively.
Chronic trauma can lead to corns and calluses of the sole. This can be treated by paring of the skin or local applications. Large calluses may need to be excised.
Inflammatory degenerative conditions that affect the foot include osteoarthritis, rheumatoid arthritis and gout. Osteoarthritis is normally secondary to trauma. Gout normally affects the big toe. Acute gouty attacks are treated with anti-inflammatory medications and rest. Long-term treatments include diet manipulation and allopurinol.
Heel pain is a frequent complaint. It is frequently due to plantar fasciitis, an inflammatory ailment involving the soft tissue around the heel. Treatment with anti-inflammatory medications, heel cushion or corticosteroid injections normally work. Surgery for plantar fasciitis has unpredictable results.
Achilles tendinitis is an inflammatory condition of the Achilles tendon. Anti-inflammatory medications and physiotherapy is the mainstay of treatment. Corticosteroid injection for achilles tendinitis is risky as it may predispose to rupture of the tendon.
Ingrown toenail infection is a common infective condition. It can normally be prevented by proper nail care. If antibiotics fail to control the infection, surgical resection of the nail may be needed.
Diabetic patients are particularly prone to infection of the foot due to reduced resistance and insensitivity of the foot due to involvement of the nerves. Amputation is always a possibility in diabetic patients.
Proper foot care involves understanding and prevention of the above ailments. Proper footwear is of utmost importance. The shoe should be comfortable to wear and support the foot at the correct places. Tight shoes and heels (although fashionable) should be avoided.
Maintaining an ideal body weight and prompt and proper treatment for injuries will prevent osteoarthritis.
Dietary manipulation to reduce purine intake is important in patients with gout to prevent the complications of hyperuricaemia.
The foot is the bane of the diabetic patient. Because of nerve involvement, their feet become insensitive and they are often unaware of something amiss until the infection is advanced. Diabetic patients should be extra vigilant of their feet. A podiatric service is invaluable.
- This article is contributed by The Star Health & Ageing Panel, which comprises a group of panellists who are not just opinion leaders in their respective fields of medical expertise, but have wide experience in medical health education for the public. The members of the panel include: Datuk Prof Dr Tan Hui Meng, consultant urologist; Dr Yap Piang Kian, consultant endocrinologist; Dr Azhari Rosman, consultant cardiologist; A/Prof Dr Philip Poi, consultant geriatrician; Dr Hew Fen Lee, consultant endocrinologist; Prof Dr Low Wah Yun, psychologist; Dr Nor Ashikin Mokhtar, consultant obstetrician and gynaecologist; Dr Lee Moon Keen, consultant neurologist; Dr Ting Hoon Chin, consultant dermatologist; Assoc Prof Khoo Ee Ming, primary care physician. For more information, e-mail [email protected]The Star Health & Ageing Advisory Panel provides this information for educational and communication purposes only and it should not be construed as personal medical advice. Information published in this article is not intended to replace, supplant or augment a consultation with a health professional regarding the reader’s own medical care.The Star Health & Ageing Advisory Panel disclaims any and all liability for injury or other damages that could result from use of the information obtained from this article.